If getting your normal brand of contraceptive pill has proven difficult these past few months it may not just be because of the coronavirus pandemic, contraceptive pill shortages have been a pandemic in itself for some months now. More and more women are facing difficulties getting access to their regular form of contraception, ‘the pill’, as it’s known. This is something which many women have been using for years without any problems.
In the past year, doctors, pharmacists, and patients alike have raised concerns about the lack of contraceptive pill supplies, as well as other forms of contraception such as the injection, and drugs to treat symptoms of menopause known as HRT. For many people, these medicines are vital for not only preventing unwanted pregnancies, but also giving some women a better quality of life as the pill is also used to treat severe symptoms of premenstrual syndrome (PMS), endometriosis, it also helps to regulate periods and make them less painful, and it can treat conditions such as acne.
So why is such an important drug suddenly becoming difficult to get hold of, and what should you do if you find that your normal form of contraception is no longer available? We spoke to our doctors about why this is a problem, what to do about it, and the alternative contraception options that you may not be familiar with.
Why is there a shortage of contraceptive pills?

A shortage of certain brands of contraceptive pill was notified last year in 2019, and we’re still seeing shortages today. Frustratingly, it’s not clear why these shortages are happening but medicine shortages are usually the result of problems in the production of certain drugs, if there’s a problem with one ingredient this can impact the supply of many different brands. It’s also been suggested that the uncertainties of Brexit could’ve been a cause of these shortages, and now the impact of coronavirus has meant disruptions in production, possibly even a complete halt in production as some factories close due to the pandemic, all of which has a knock-on effect on the supply here in the UK.
However, the NHS naturally experiences temporary shortages from time to time and they’re well equipped to deal with shortages.
Norimin, Noriday, Synphase, Brevinor, Loestrin, Zoely, and Cilest are just some of the popular brands of contraceptive pill that have been in short supply at some stage over the past year.
How do these shortages affect patients?
A temporary shortage in any medicine can have a huge impact on a patient’s mental and physical wellbeing. Not being able to get hold of your normal contraceptive pill is not only inconvenient, but it also risks unwanted pregnancies, unnecessary abortions, and for those who are using the pill for other means such as to reduce the debilitating symptoms of PMS, a shortage can really reduce a person’s quality of life. Patients are often not informed that their pill is out of stock until they go to collect it from the pharmacy which can often be when the patient has finished their pack and has no pills left, this leaves the patient in a difficult and distressing situation.
What should you do if your pill is not available?
If you’ve been told that your contraceptive pill is out of stock or completely discontinued it’s likely that you will have been offered an alternative pill. Your doctor will offer an alternative pill that has the same or similar ingredients as your original pill, which sounds ideal, right? For some women, it will be no bother switching to another pill, however, there is a risk of side effects when switching pills, particularly in the first 3 months.
Switching to a new pill is not so plain sailing for some women as nausea, breakthrough bleeding, and mood changes are some of the side effects that are experienced when starting a new pill. Plus, switching to a new pill is a risky time for pregnancy to occur, you’ll need to use a backup method of contraception such as condoms for the first week or even month of starting your new pill to be on the safe side, speak to your doctor about how long you should be using backup methods for while your body adjusts to this new pill.
Your doctor should look at the closest match to the pill that you’re used to by taking into account dose, strength, and the key ingredients in your pill. Finding the right pill can be trial and error so if this new pill isn’t working for you go back to your doctor to find an alternative.
Is the pill the only effective contraceptive available?
Absolutely not, there are many more methods of contraception that are just as effective as the combined and mini pill and may be more suited to you. Many people aren’t aware of the array of contraceptives out there and automatically assume that the pill is the best option for them. While the contraceptive pill is very popular and highly effective, there is no harm in exploring other options.
We’re going to talk you through each of these options and their pros and cons.
The contraceptive pill

The pill is a classic contraceptive that was revolutionary for women’s sexual freedom when it was introduced in the 1960s, and it’s still the most popular and commonly used method to prevent pregnancy. Although it has had criticism over its safety (read more about that here) it’s still as popular as ever.
There are two types of contraceptive pill, the combined pill, and the mini pill. The combined pill contains artificial versions of natural female hormones known as oestrogen and progesterone and it works to prevent pregnancy by stopping the release of an egg (ovulation) or by stopping an egg from being fertilised by sperm. The combined pill is usually taken every day for 21 days and then there is a 7-day pill break when you will have a period-type bleed and you are still protected against pregnancy during this time.
The ‘mini pill’, otherwise known as the progesterone-only pill, works in the same way as the combined pill to prevent pregnancy, but it contains one hormone (progesterone) instead of two so it’s suitable for women who can’t take pills containing oestrogen. The other difference between the combined pill and the mini pill is that the mini pill is taken every day with no break between the packs of pills.
The pill is over 99% effective which is why it’s so popular.
| The Pill | |
| Pros | Cons |
| Over 99% effective at preventing pregnancy | May cause some side effects particularly in the first 3 months such as nausea, breast tenderness, headaches, and mood swings |
| Doesn’t interrupt sex | Can increase blood pressure - you should have your blood pressure monitored every 3-6 months |
| Easy to take (if you’re ok with remembering to take pills) | Does not protect against STIs as barrier methods do such as condoms |
| Makes periods more regular, lighter, and less painful | You may experience breakthrough bleeding or spotting |
| Reduces symptoms of PMS | The pill has been linked to blood clots (thrombosis) |
| May reduce acne | You need to remember to take it every day |
| It may protect against pelvic inflammatory disease | Not suitable for women over the age of 35, those who smoke, or those who have certain medical conditions |
| Research has shown it may reduce the risk of ovarian, colon, and womb cancer | |
| Research suggests it may reduce the risk of fibroids, ovarian cysts, and non-cancerous breast disease | |

The contraceptive patch

The patch looks a bit similar to the stop smoking patch, it’s a small sticky patch that you put on your skin and it releases the same hormones that are in the combined pill into the bloodstream to prevent pregnancy. Again, you have a 7-day break after wearing the patch for three weeks but you will need to change the patch once a week. It’s over 99% effective so it’s just as effective as the pill but you don’t need to think about it as often.
The patch can be applied to any part of your body apart from your breasts, or anywhere that is hairy, and it shouldn’t be applied to sore or irritated skin. It may be visible depending on where you put it but you can be discreet with it if you want to as long as it’s not covered by tight clothing which may rub it off.
| The Patch | |
| Pros | Cons |
| Over 99% effective at preventing pregnancy | May cause some side effects particularly in the first 3 months such as nausea, breast tenderness, headaches, and mood swings |
| Doesn’t interrupt sex | May experience skin irritation, itching, or soreness |
| Easy to use and you only have to think about it once a week to change it rather than daily | Does not protect against STIs like barrier methods do such as condoms |
| Hormones aren’t absorbed by the stomach so if you vomit or have diarrhoea your patch will still work. If this happens while taking the pill it’s less effective and you will need to take another pill | You may experience breakthrough bleeding or spotting |
| Makes periods more regular, lighter, and less painful | The patch has been linked to blood clots (thrombosis) |
| Reduces symptoms of PMS | You need to remember to change it once a week |
| Research has shown it may reduce the risk of ovarian, colon, and bowel cancer | Not suitable for women over the age of 35, those who smoke, or weigh 14 stone or more |
| Research suggests it may reduce the risk of fibroids, ovarian cysts, and non-cancerous breast disease | Some medicines may make it less effective |
The contraceptive ring
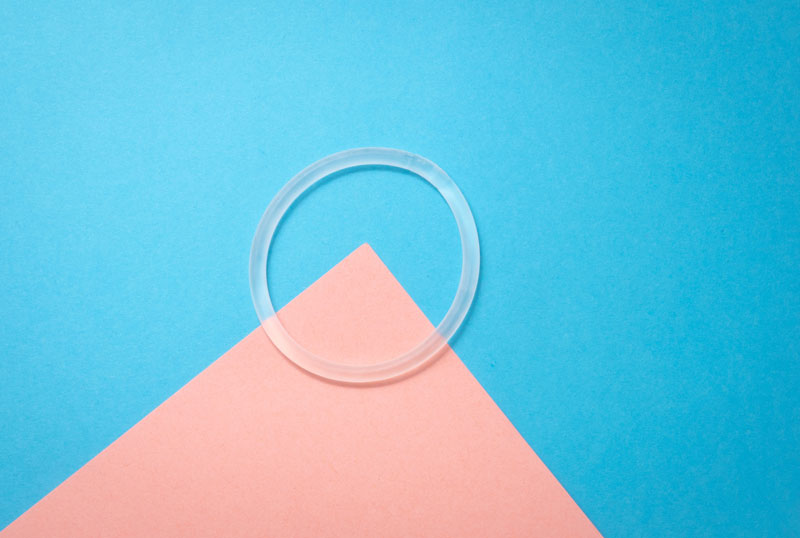
The contraceptive ring or the vaginal ring may not be used as widely as the pill but it’s certainly one to consider given that it’s more than 99% effective. The biggest benefit of this form of contraception is that it provides contraception for a whole month without having to think about it every day. The ring is inserted into the vagina and it releases progesterone and oestrogen hormones into the body to prevent ovulation and fertilisation. The ring is left in your vagina for 21 days and then it is taken out for a 7-day break which is when you may have a period-type bleed, but you’re protected against pregnancy for the entire 28 days.
You can still have sex while the ring is inside you.
| The Ring | |
| Pros | Cons |
| Over 99% effective at preventing pregnancy | May cause some side effects particularly in the first 3 months such as increased vaginal discharge, nausea, breast tenderness, headaches, and mood swings |
| Doesn’t interrupt sex | Does not protect against STIs like barrier methods do such as condoms |
| Easy to use and you don’t have to think about it each day or every time you have sex | You may experience breakthrough bleeding or spotting |
| The ring isn’t affected by vomiting diarrhoea so you will still be protected against pregnancy | You need to remember to remove it and change to a new one each month |
| Makes periods more regular, lighter, and less painful | Some people may not be comfortable inserting and removing the ring |
| Reduces symptoms of PMS | Not suitable for women aged 35 or over, those who smoke, are overweight or have certain health conditions |
| Research has shown it may reduce the risk of some cancers | Some medicines may make it less effective |
The contraceptive injection

This one might sound a little daunting but it’s one of the quickest, easiest, and long-lasting methods of contraception. The injection lasts for 8 or 13 weeks depending on the type of injection and it prevents pregnancy by releasing progesterone into the bloodstream. Depending on the type of injection it’s usually administered by your nurse or GP in either your bottom, thigh, abdomen or upper arm.
This option is good for those who want contraception that lasts longer than the other methods mentioned above. If you’re at a stage where you know you don’t want to be pregnant for at least a year then the injection may be a hassle-free way of achieving this as it can take up to one year for your fertility to return to normal. Again, as with the other methods it works by stopping ovulation and fertilisation of an egg to prevent pregnancy occurring.
| The Injection | |
| Pros | Cons |
| Over 99% effective at preventing pregnancy | May cause some side effects such as acne, hair loss, decreased sex drive, nausea, breast tenderness, headaches, and mood swings. These side effects may last for your entire course and after |
| Doesn’t interrupt sex | Does not protect against STIs like barrier methods do such as condoms |
| Last for 8 or 13 weeks | It can alter your periods and this can last for some months after stopping the injections |
| Easy to get at your GP or clinic and you don’t have to think about it each day or every time you have sex | It can be up to one year before your periods and fertility return to normal |
| Safe to use while breast-feeding | May cause weight gain in some people |
| Suitable for those who can’t use oestrogen-based contraceptives | Not suitable for women who have certain health conditions |
| Not affected by other medicines | |
| Can make periods more lighter, and less painful | |
| May reduces symptoms of PMS | |
The contraceptive implant

Moving onto the more long-lasting methods of contraception, the implant is a small, plastic device that is placed under the skin in your upper arm and releases progesterone in the body to prevent pregnancy for up to 3 years. It’s highly effective and is great if you’re planning to not get pregnant for at least another 3 years but want your fertility to return quite quickly after this time, and you can have it removed at any time if your plans change. Remember that once you’ve had the implant taken out you won’t be protected against pregnancy.
Getting the implant inserted by your GP or nurse is quick and with minimal pain as a local anaesthetic is used to numb the area.
| The Implant | |
| Pros | Cons |
| Over 99% effective at preventing pregnancy | May cause some side effects in the first few months such as nausea, breast tenderness, headaches, and mood swings |
| Doesn’t interrupt sex | Does not protect against STIs like barrier methods do such as condoms |
| Long lasting - lasts for 3 years | It can alter your periods making them irregular or stop altogether |
| Easy to get at your GP or clinic and you don’t have to think about it each day or every time you have sex | You may develop acne or your acne may become worse |
| Safe to use while breast-feeding | You’ll need to have small, minor procedure to have the implant fitted |
| Suitable for those who can’t use oestrogen-based contraceptives | Not suitable for women who have certain health conditions |
| Can reduce painful and heavy periods | Certain medicines may make the implant less effective |
| Your fertility will return to normal as soon as you have the implant taken out | |
The Intrauterine device (IUD) or the Intrauterine system (IUS)

The IUD and IUS are the most long-lasting but not permanent methods of contraception that we’ve mentioned. They’re a T-shaped device that is made of plastic, but the IUD is made of plastic and copper and it’s inserted into your womb by your doctor. You may have also heard the IUD be referred to as the ‘coil’ or the ‘copper coil’ as it works by releasing copper to prevent pregnancy for 5 to 10 years, whereas the IUS releases the hormone progesterone to prevent pregnancy for 3 to 5 years. They’re both more than 99% effective and they work by thickening the cervical mucus to make it difficult for the sperm to reach the egg and fertilise it and can also stop a fertilised egg from implanting.
Although the initial procedure can be uncomfortable and isn’t without its risks, it’s a method of contraception that doesn’t have to be thought about for at least 3 to 5 years.
| The IUD | |
| Pros | Cons |
| Over 99% effective at preventing pregnancy | May cause some uncommon side effects in the first few months such as vaginal bleeding or pain |
| Doesn’t interrupt sex | Does not protect against STIs as barrier methods do such as condoms |
| Long-lasting - lasts for 5 to 10 years | Periods may become heavier, longer-lasting, and more painful |
| Don’t have to think about it each day or every time you have sex | Risk of infection when the IUD is fitted which may lead to pelvic infection |
| Safe to use while breast-feeding | You’ll need to have a quick procedure which may be uncomfortable but you can have a local anaesthetic |
| Can be used by most women - suitable for those who can’t use oestrogen-based contraceptives and those who have migraines | You may experience period-type cramping after the procedure but painkillers can ease this |
| Works straight away once fitted | Not suitable for women who have certain health conditions |
| Your fertility will return to normal as soon as it’s removed | |
| Not affected by other medicines | |
| No hormonal side effects | |
| The IUS | |
| Pros | Cons |
| Over 99% effective at preventing pregnancy | May cause some side effects in the first few months such as acne, breast tenderness, headaches, and mood changes, or vaginal bleeding or pain, but this is less common |
| Doesn’t interrupt sex | Does not protect against STIs as barrier methods do such as condoms |
| Long-lasting - lasts for 3 to 5 years | It can alter your periods making them irregular or stop altogether |
| Not affected by other medicines | Risk of infection when IUS is fitted which may lead to pelvic infection |
| Safe to use while breast-feeding | You’ll need to have a quick procedure which may be uncomfortable but you can have a local anaesthetic |
| Suitable for those who can’t use oestrogen-based contraceptives | You may experience period-type cramping after the procedure but painkillers can ease this |
| Periods may become lighter and less painful | Not suitable for women who have certain health conditions |
| Your fertility will return to normal as soon as you have the IUS removed | |
The contraceptive diaphragm or cap

If committing to a long term contraceptive method is not for you then the use of a diaphragm or cap may be more suited to you. It’s the least effective of all the methods we’ve mentioned but it’s still pretty effective at 92-96%. The great thing about this method is that there are no serious health risks, it’s something that you use each time you have sex, so if you don't mind a bit prepping before sex then this is ideal for you.
As I said, there is a bit of prepping and thinking that goes into this one as you’ll need to insert it into your vagina before you have sex and then leave it in for 6 hours after sex, and it needs to be used with spermicide (a gel that kills sperm). You’ll need to apply more spermicide each time you have sex. Although it’s a barrier method of contraception don’t be fooled into thinking that this totally protects you from sexually transmitted infections as it’s not as reliable as condoms. To protect against pregnancy and STIs use a condom as well as the diaphragm or cap.
Once you get used to how it works, each time you use it will become much easier and more routine.
| The Diaphragm or Cap | |
| Pros | Cons |
| Only needs to be used when you want to have sex | Does not reliably protect against STIs as other barrier methods do such as condoms |
| No serious health risks or side effects | Not the most effective contraception |
| Puts you in control of your contraception | Takes time to learn and get used to it |
| May interrupt sex | |
| Risk of cystitis (bladder infection) | |
| You or your sexual partner may experience irritation from the latex or spermicide | |
| Not suitable for women who have certain health conditions | |
Male and female condoms

Last and by no means least are condoms, these are highly effective at protecting against pregnancy and STIs and are often used in combination with other contraceptives for their double protection. Condoms are a barrier method of protection which means it stops the sperm from reaching the egg. Male condoms are more effective at 98% compared to female condoms which are 95% effective and they’re more widely available than their female counterparts.
|
Condoms |
|
|
Pros |
Cons |
| Only needs to be used when you want to have sex |
Some people may find it interrupts sex |
| No serious health risks or side effects | Although condoms are strong, if they’re not used properly they may split or tear |
| Puts you in control of your contraception | You or your sexual partner may experience irritation from the latex or spermicide, however, there are alternative condoms which cause less irritation |
| Highly effective at preventing pregnancy if used correctly | |
| Protection against sexually transmitted infections | |
Contraception that suits you
Contraception is entirely your choice, and this post just goes to show that if your current contraception isn’t working for you or is no longer available, there are many more to choose from. Don’t be disheartened if you find that one method or the most commonly used method isn’t working for you, speak to your GP about it and discuss any of the methods we’ve mentioned here, plus any others that may be available to you.
Our contraception section also has lots of information on this too, and if you’ve found one that works, they’re available to buy conveniently, safely, and discreetly at Doctor 4 U.
Emergency contraception

If you feel that your contraception has failed or you've forgotten to take, use, or renew your regular form of contraception, maybe you've accidentally had sex without using any contraception at all, then emergency contraception is an option to prevent pregnancy from happening. Emergency contraception, as the name suggests, should only be used occasionally in emergencies and not as your regular contraception. Emergency contraceptive pills work in the same way as the contraceptive pill but it's at a higher dose which is why it's not recommended to be taken regularly. Depending on which brand you use, emergency contraception can prevent pregnancy occurring after unprotected sex for up to 5 days, but the sooner you take it the more effective it is.
Emergency contraception is often mistaken for an 'abortion pill' but this is not the case as it cannot stop pregnancy once it has occurred but it can prevent this happening, however, this is not always guaranteed. Again, this type of contraception needs to be taken as soon as possible after unprotected sex and you can get it urgently at any of the below services:
- Most walk-in centres/ Minor injuries units
- Contraception clinics
- Brook centres
- Some pharmacies
- Most GUM clinics
- Most GP surgeries
You can find emergency contraception services in your area on the NHS website. If it's not possible to get to these places you can order emergency contraception online here at Doctor 4 U. We offer next day delivery so you could have your emergency contraception tomorrow. We've also answered all the questions you may have about emergency contraception in the link below:











