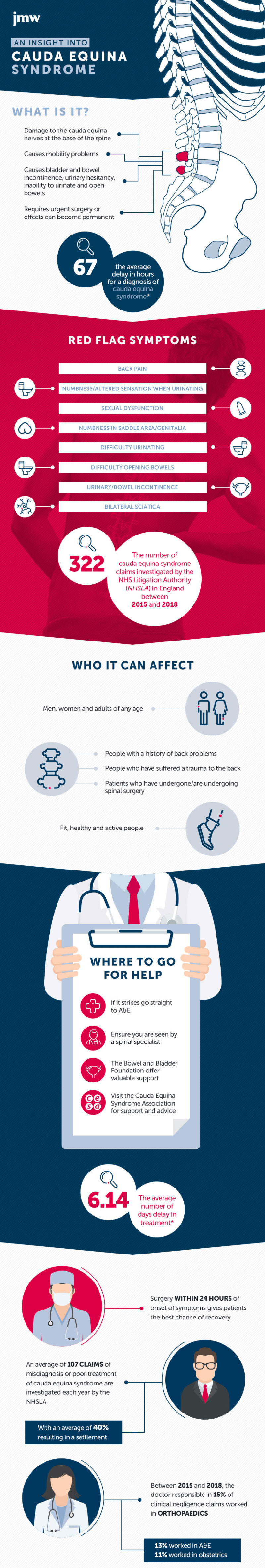
What is Cauda Equina Syndrome?
Cauda Equina Syndrome is a rare but extremely serious condition. It is classified by the compression of the lumbar (low back) spinal cord which contains a large group of nerves. In this part of the spine, the nerves branch together and appear similar to a horse’s tail, hence its name; Cauda Equina.
When the cauda equina becomes impacted, problems begin to arise.
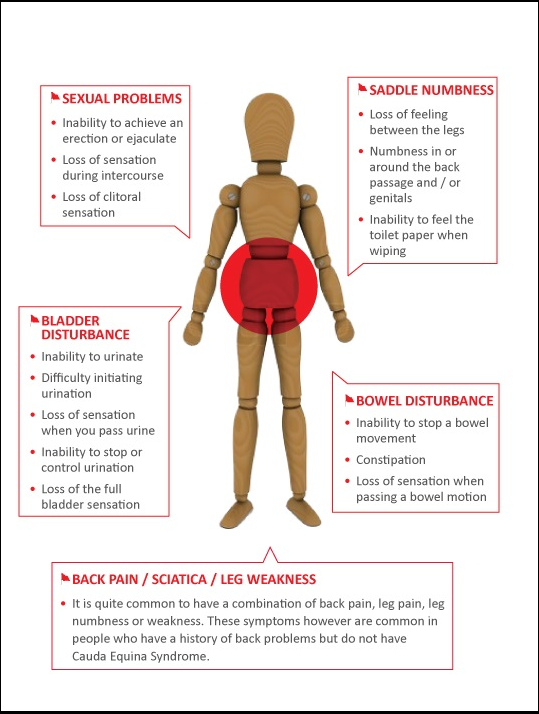
Depending on the severity of the nerve compression, these symptoms may be present:
- Back pain
- Bilateral pain
- Sciatica
- Saddle numbness
- Leg weakness/numbness
- Incontinence
- Bladder and/or bowel disturbances
Whilst some of these symptoms may only describe a bulging disc or trapped nerve, the combination of pain and saddle anaesthesia/incontinence along with altered sensation in the legs is a red-flag combination, and requires emergency treatment.
Compression of the spinal cord can be caused by a herniated disc, bone (either fragments or spurs, or a condition called spondylolisthesis [spondy-low-lis-thee-sis]), tumours or growths, or anything else that might impact the nerves.
Cauda Equina Syndrome can either happen suddenly or gradually and unfortunately, there isn’t a way to prevent it from happening to you. However, the condition is rare, so if you do experience back pain, you shouldn’t immediately panic. Seek medical advice and note down all of your symptoms.
Credit: The Cauda Equina Syndrome Foundation (CESA)
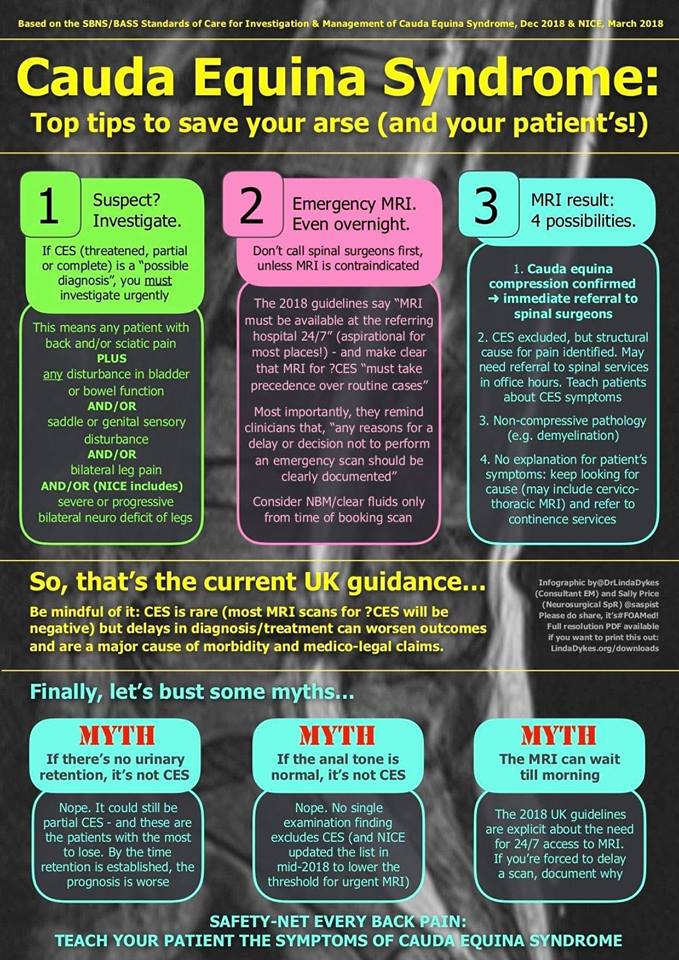
How is Cauda Equina Syndrome diagnosed?
If a patient is displaying symptoms of CES, a doctor should first perform a physical examination to check sensation in the legs, as well as enquiring about saddle numbness and bowel & bladder changes.
If the doctor then suspects that a patient might be at risk of developing or even already having CES, an MRI scan should be performed at the soonest possible opportunity. The MRI will show the spinal cord in more detail than an X-Ray, and the compression severity and cause should be able to be determined from the resulting images.
How is Cauda Equina Syndrome treated?
In a vast majority of cases, CES requires urgent surgery to remove the compression of the spinal cord. Many patients will still require treatment to manage their symptoms afterwards. In most cases, neuropathic pain relief is given long-term, such as amitriptyline, gabapentin or pregabalin. Some patients may need more traditional pain relief, like opioid treatments such as co-codamol, or a strong NSAID such as naproxen.
Whilst in many cases, nerve damage can’t be reversed, these treatments generally help to reduce the symptoms and improve the quality of life for patients that suffer, even after their operation.

Real-life story
Ellena, 24, recalls when she went to her GP complaining of bilateral pain, numbness, and bladder disturbances:
“I was 22 when I first started to notice symptoms of CES. I’d struggled with a bad back for a few years, but the symptoms suddenly started to get worse without any real reason. I first noticed sciatic pain in my right leg, so I went to my GP for advice. They told me it could last 6 weeks and would probably go away on its own, so I was given painkillers"
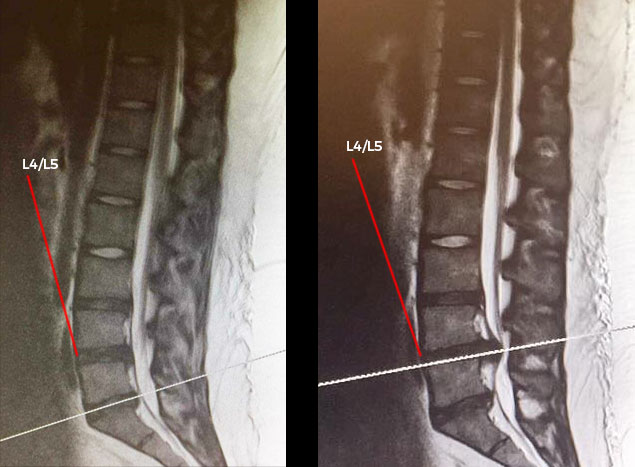
Left: Ellena's MRI scan from 2016, showing a slight bulge at L4/L5
Right: Ellena's MRI scan from 2017, showing a severe herniation compressing the cauda equina at L4/L5
When did you know something was seriously wrong?
The pain didn’t improve with the painkillers, and over the course of a few weeks, it got much worse. I remember having excruciating pain in both legs that felt like rubber bands being stretched as far as they could before snapping. One night, I had some disturbances to my bladder function, but because I wasn't sure if it was a red-flag symptom, I kind of ignored it. The next morning, I couldn’t move my legs. My mum had to help me out of bed to go to the toilet, but my legs just weren’t waking up.
What did you do next?
I had a telephone consultation with my GP surgery. By this time I was in agony, and despite the debilitating pain in my legs, I also had some degree of numbness. I told my doctor about my symptoms, including the bladder disturbance, and they told me to take the painkillers”
What changed for you to eventually be diagnosed?
After I returned from a trip, I had to take some time off sick from work. By this time, I couldn’t walk without support anymore, and I slowly hobbled into the doctor’s office on crutches. It was a different GP to the one I’d seen and spoken to previously, and he recognised that I wasn’t just suffering from a bad back. He referred me to a neurosurgeon who then arranged for an MRI. The day after my scan, I was asked to go back to the hospital as soon as possible and under no circumstances should I drive myself there.
My parents and I arrived in the evening to be told that I had a very serious spinal cord compression that needed urgent surgery or else I’d risk permanent paralysis.
How did you react to the news?
I burst into tears in shock. I was also a bit relieved that it wasn’t all in my head and that someone was finally going to make it better. I was terrified about the surgery, though. It was my first operation and there was no guarantee that it would solve the problem, as the nerves could have been so badly damaged that I could have lasting symptoms.
After my operation, I was taken into another hospital with severe back pain, where another consultant told me that the symptoms I'd had prior to the operation clearly indicated Cauda Equina Syndrome.
And do you?
Yes, but nothing too serious. I see stories all the time of others that have been through the same thing, and they have to self-catheterise. I still get back pain, and I have some left-over neuropathic symptoms. My right leg which was the worst affected one will sometimes just go totally numb, especially in winter. But other than that, I’m really thankful that I can walk and drive again. It does get me down sometimes, but others have it so much worse. I sometimes have to use crutches and take strong painkillers, and there are certain things I can't do anymore. I've lost some of my mobility, but I make the most of what I've got. I'm lucky that my injury wasn't complete, as some people that experience complete compression of the spinal cord end up with paralysis.
What do you want others to know?
Because it’s such a rare syndrome, so many people aren’t aware of the red flag symptoms and brush it off as a bad back. I’d like people to know what to look out for, and that if they experience any numbness or bowel and bladder changes to seek emergency treatment.
Also, living with the aftermath of such a major spinal cord injury is something that can be quite difficult. Depending on the pain flare-ups, it can be difficult to go about your day-to-day life. Many rare diseases and conditions are invisible, so I’d also like people to realise that some impairments and disabilities aren’t obvious. The sunflower lanyard initiative that has been adopted by many UK airports is a great idea to show people that you have a hidden disability or impairment. It’d be fantastic to see this implemented in other areas too.
Credit: Linda Dykes @DrLindaDykes (Twitter) Sally Price @saspsit (Twitter)
Credit: JMW Solicitors











Thanks Debra ?
All the best,
Doctor4U